The human skeletal-muscular system contains highly trainable tissue that can be remarkably effective in managing glycemic control, which in turn helps manage or prevent type 2 diabetes. Hurley, Hanson and Sheaff (2011) note that muscular strength is inversely related to metabolic syndrome, a cluster of risk factors leading to the development of type 2 diabetes and cardiovascular disease. The researchers add that high insulin levels, low muscle mass and low strength are the strongest factors associated with increased risk of metabolic syndrome.
Ishiguro et al. (2016) explain that muscle contraction leads to a variety of muscle cell responses that ultimately enhance glucose uptake. Resistance exercise promotes glucose utilization by raising the number of glucose transporter-4 (GLUT4) proteins (transporter proteins taking glucose into muscle cells); by producing more insulin receptors; and by increasing the activity of protein kinase B (a signaling protein) and glycogen synthase (an enzyme involved in converting glucose to glycogen) (see Figure below).
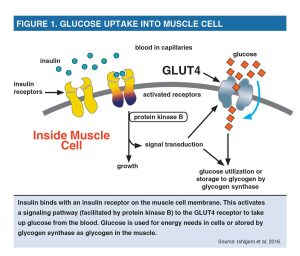
Muscle contraction reduces blood glucose concentrations and increases insulin sensitivity during and after exercise, with enhanced insulin sensitivity persisting for up to 24 hours (Colberg et al. 2010). Resistance exercise increases glucose uptake by upregulating (increasing the response to) the GLUT4 transporters, which can travel from within the cell to the membrane in response to muscle contraction (Gordon et al. 2009). The increased uptake moves glucose out of the blood and into the muscle, where it is used for energy needs or stored as glycogen for future exercise or work use.
Maximizing Activated Muscle Mass
Given that the glucose response is specific to the contracting muscles, Ishiguro et al. (2016) suggest focusing on exercises that will increase the muscle mass to be activated. To optimize glucose uptake, symptomatic people should do resistance exercises that engage large muscles and/or multiple muscle groups. The larger the muscle mass activated, the greater the potential for exercise-induced glucose uptake, because more GLUT4 transporters and insulin receptors will be stimulated.
What Are Hemoglobin A1C (HBA1C) and EAG?
Hemoglobin, the oxygen-carrying protein inside a red blood cell, sometimes joins with the glucose in the bloodstream—a process called glycation. As glucose in the blood rises, more hemoglobin becomes glycated. The designation “hemoglobin A1c” (the “A” stands for adult, and the “1c” is the component on hemoglobin that the glucose binds to) provides an average of blood sugar control over the previous 2–3 months. This data point and daily monitoring are used to adjust a person’s diabetes medicines and lifestyle.
HbA1c is reported as a percent (e.g., 7%). The eAG, or estimated average glucose, is similar to the unit used to self-monitor blood glucose. The eAG uses the same units (milligrams per deciliter) as a glucose meter. As with HbA1c, the eAG shows the average blood sugar over the previous 2–3 months. To convert HbA1c to eAG, use this formula: 28.7 x HbA1c – 46.7 = eAG (in mg/dL).
- The normal range for the hemoglobin HbA1c test for those without diabetes is between 4% and 5.6%.
- Hemoglobin A1c levels between 5.7% and 6.4% signify prediabetes, meaning people are at an increased risk of type 2 diabetes.
- A HbA1c of 6.5% or higher means the person has diabetes.
- The goal for people with diabetes is a hemoglobin A1c below 7%.
Source: Adapted from “Resistance Training and Diabetes”, by Kurt Escobar, MA and Len Kravitz, PhD, IDEA Fitness Journal, Mar 13, 2016